DSEK: Sutureless Corneal Transplant In NYC
Dr. Gregory Pamel is a highly skilled cornea transplant surgeon who has helped many New York area patients regain excellent vision. In the paragraphs below Dr. Pamel describes the new DSEK sutureless corneal transplant procedure and how the procedure can be used to treat New York corneal transplant patients.
DSEK (Descemet Stripping Endothelial Keratoplasty) is a new option for patients with corneal edema who require corneal transplantation. This procedure has several advantages over traditional corneal transplant surgery which include:
- Faster visual recovery
- Less astigmatism created since there are no sutures
- Eye is much stronger and more resistant to injury since only the diseased tissue rather
- than the entire cornea is replaced.
- Surgery time is quicker
- Chance of rejection is reduced significantly
- Procedure can be combined with cataract surgery
In order to understand this new procedure one must understand the conditions and pathology that lead to corneal edema.
The back cellular layer or posterior layer of the cornea is called the endothelium and is responsible for maintaining the clarity of the cornea by pumping excess fluid from the cornea. The endothelium has a finite number of cells; that is these cells are unable to be replaced once they are damaged or die. Certain conditions can cause loss of these finite cells (endothelial cell loss) leading to corneal edema and vision loss. Irreversible corneal edema occurs when the endothelial cell loss occurs to such an extent that fluid is no longer able to be pumped from the cornea and the cornea swells preventing light from being focused on the retina.
Endothelial Cell Loss Causes
There are two main conditions which result in irreversible endothelial cell loss:
Pseudophakic Bullous Keratopathy – Corneal Edema (swelling)
This is a condition in which one’s cornea has become permanently swollen (corneal edema) following cataracts and intraocular lens implant procedure. The cells that line the back inside surface of the normally crystal clear cornea (the endothelium), for one of various reasons, have been injured permanently. The function of the endothelium is to pump water out of the cornea, keeping it crystal clear and thin. When injured, these cells can no longer perform this function. The fluid that circulates inside the eyeball seeps into the cornea, causing it to swell and to become cloudy. This condition is called pseudophakic bullous keratopathy.
The causes of endothelial cell damage following cataract operations are multiple. They include physical trauma during the operation, such as difficulties in removing the cataract or inserting the intraocular lens, severe inflammation following the operation, intraoperative bleeding, or a predisposing disease called Fuchs’ endothelial dystrophy that makes the cornea prone to losing endothelial cells. When one is afflicted with pseudophakic bullous keratopathy, the cornea is permanently swollen and no medications, spectacles, or contact lenses can improve the vision of a patient with this condition.
Fuchs’ Endothelial Dystrophy
The normally crystal clear cornea has a layer on its inside surface called the endothelium. The purpose of this layer of cells is to pump water out of the cornea keeping it crystal clear and thin. Normally, as we age, these cells can become thick and fat. When the ophthalmologist looks at your eyeball through the slit lamp microscope, these cells can be detected and are termed guttata. Guttata are part of the normal aging process of the corneal endothelium.
Fuchs’ endothelial dystrophy was first described more than 100 years ago. It is a process in which guttata occur throughout the entire back surface of the cornea and appear one to three decades earlier than is normally expected.
In Fuchs’ endothelial dystrophy, as the guttata increase in size and numbers, fluid begins to accumulate within the cornea. Patients develop blurry or foggy vision in the morning, see halos around lights early in the morning, are unable to read in the early part of the day, etc. As the day goes on and the cornea dehydrates on its own, it becomes clearer and thinner and the patient’s vision improves. As the process of Fuchs’ endothelial dystrophy progresses, the swelling of the cornea persists further on into the day until eventually the vision never clears.
Surgical Treatment of Pseudophakic Bullous Keratopathy & Fuch’s Endothelial Dystrophy using the DSEK procedure:
In both pseudophakic bullous keratopathy and Fuch’s dystrophy, only the endothelium is diseased-the remaining layers of the cornea are usually normal and healthy. Until recently, the treatment of choice in patients with corneal edema from endothelial cell loss was a corneal transplant operation (penetrating keratoplasty). This involves replacing the entire cornea using a full thickness donor cornea. Recently a new procedure was developed to treat this condition called DSEK. DSEK stands for Descemets’ stripping endothelial keratoplasty. In this procedure, the damaged endothelium is stripped and removed from the patient’s eye and replaced with a partial thickness piece of donor cornea containing a healthy endothelium (posterior graft). Dr. Pamel was one of the first people in New York to perform this technique on patients.
This procedure is done through a sutureless incision and therefore results in a faster visual recovery. Most patients recover useful vision (20/60 or better) within three months of surgery compared to a full thickness corneal transplant which may take up to a year or longer to achieve the same level of vision. Dr. Pamel no longer recommends performing a standard corneal transplant on most patients with pseudophakic bullous keratopathy or Fuch’s dystrophy unless they significant corneal scarring.
DSEK Procedure Details
- The patient’s endothelial layer is stripped from the rest of the cornea.
- The donor endothelium attached to a thin layer of donor cornea is folded like a taco and inserted through a 5mm incision.
- An air bubble is injected to push the donor cornea up against the posterior surface of the patient’s cornea.
- The pumping action of the new donor endothelium helps to create suction which bonds the donor tissue to the patient’s own cornea
Advantages of DSEK/Sutureless Corneal Transplant
- Visual recovery is significantly faster.
- The eye is left much stronger and more resistant to injury.
- Suture related complications are essentially eliminated.
- There is little or no change in the refractive error since the patient’s cornea is left intact.
Complications of the DSEK Procedure:
The posterior graft can dislocate and may need to be repositioned or replaced. In some instances a regular corneal transplant may need to performed.
DSEK FAQ
What’s the Difference Between DSEK and DMEK Surgery for Corneal Transplant?
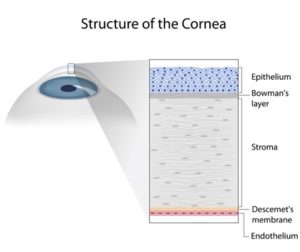 DSEK and DMEK procedures are partial thickness corneal transplants that replace the innermost corneal sections. They are similar procedures, except the Descemet’s membrane endothelial keratoplasty (DMEK) procedure does not include stromal tissue in the implanted donor material. DMEK is a thinner graft (15-20 microns) than DSEK because it is a pure endothelium replacement. DSEK may offer a slightly shorter and easier recovery with fewer days of lying flat, but DMEK has a lower donor graft rejection rate (1 percent versus 10 percent).
DSEK and DMEK procedures are partial thickness corneal transplants that replace the innermost corneal sections. They are similar procedures, except the Descemet’s membrane endothelial keratoplasty (DMEK) procedure does not include stromal tissue in the implanted donor material. DMEK is a thinner graft (15-20 microns) than DSEK because it is a pure endothelium replacement. DSEK may offer a slightly shorter and easier recovery with fewer days of lying flat, but DMEK has a lower donor graft rejection rate (1 percent versus 10 percent).
Both procedures can offer better visual quality. Our highly skilled cornea transplant surgeon can determine which approach is best for your ocular health and visual acuity.
What Can You Not Do After a Corneal Transplant?
Make sure you don’t rub your eyes and follow post-op directions from our eye surgeon closely after your DSEK procedure. Avoid heavy lifting and strenuous exercise until you’re cleared to do so by Dr. Pamel. Stay away from dusty and smoky environments that may irritate your eyes, and wear sunglasses to ease light sensitivity. Contact sports and swimming should be strictly avoided until Dr. Pamel gives you clear instructions that it’s safe to perform these activities, and don’t forget to wear protective goggles.
Showers and baths are fine but don’t get water in the eye for the first four weeks, and don’t drive until Dr. Pamel gives you the go-ahead. Other parts of your daily routine may be off-limits for a while, so be sure to discuss your everyday tasks and job duties with our team at Pamel Vision and Laser Group.
What Should I Expect from DSEK Recovery?
 Patients who have a partial-thickness corneal transplant may go home the same day of their procedure, but a penetrating (full-thickness) keratoplasty requires an overnight stay at the hospital for monitoring. You will need to lie on your back during the first 24 to 36 hours after DSEK as much as possible.
Patients who have a partial-thickness corneal transplant may go home the same day of their procedure, but a penetrating (full-thickness) keratoplasty requires an overnight stay at the hospital for monitoring. You will need to lie on your back during the first 24 to 36 hours after DSEK as much as possible.
An eye patch is used right after surgery; you will need to wear it as directed and at night for a few weeks. You may take over-the-counter pain medications to ease your discomfort. DSEK is a suture-less corneal transplant. Steroid and antibiotic eye drops are necessary; you will need to take extra care to administer them correctly and at the right time, as explained in your post-surgical documents.
You will have blurred vision for several weeks after DSEK while your cornea heals. If you work a low-activity job such as desk work, you may return two to three weeks after DSEK, but if you have a physically demanding job you may need to take additional time off after your corneal transplant. It may take several weeks, a year or longer for your vision to stabilize after a corneal transplant, as healing varies by patient.
Dr. Pamel and our New York office staff are available to answer your questions and concerns throughout your DSEK recovery. You will have regular follow-up visits to our office in Astoria.
Why Do I Need to Lie Flat After DSEK Surgery?
You need to lie flat as much as possible for up to 36 hours following your DSEK surgery. An air bubble is used for partial-thickness transplants to keep the donated corneal tissue in place. Your eye absorbs the air bubble after a few days. You need to lie flat with your face pointing directly upward to ensure the air bubble supports the transplanted tissue floating on top. DSEK patients need to stay in this position for a day and a half, while DMEK patients must lie flat for four or five days.
When is it Safe to Drive After DSEK Surgery?
When you can drive safely after a partial-thickness corneal transplant with DSEK depends on how quickly your vision stabilizes. Many patients can see clearly and drive without concerns after two or three months. However, if you have good vision in the eye that did not receive a transplant, you may drive much sooner. Dr. Pamel can determine when your eyesight is good enough to drive safely.
Call our office today at (212) 355-2215 to schedule a consultation. For more information on Sutureless Corneal Transplant, contact our office today.





